Medical Treatment for Vitiligo
There are two types of UV treatment, namely Psoralen-UVA (PUVA) and Narrowband UVB (NB-UVB).
NB-UVB refers to a specific narrow-spectrum wavelength (311-312nm) of UVB, which has been clinically proven to treat various skin diseases such as eczema, vitiligo, and psoriasis. NB-UVB is safe and effective (suitable for pediatric patients/pregnant women/nursing women) and also meets the economic principle of convenience and time-saving. The treatment time for NB-UVB is very short (a few seconds to several minutes), reducing the overall treatment duration, and it is more effective at improving vitiligo conditions than other spectral wavelengths, while maintaining its efficacy for a longer period. It does not require the use of photosensitizing drugs, has no side effects from such drugs, and does not have the concerns of burns, photoaging damage, and skin cancer caused by PUVA.
Several international organizations concerned with vitiligo, including The Vitiligo Working Group (VWG), the American Vitiligo Research Foundation, Inc. (AVRF), Vitiligo Society UK believe that UVB is currently the safest and most effective treatment for vitiligo. The VWG (Vitiligo Working Group) has also formulated and published clinical guidelines for NB-UVB vitiligo treatment, listing recommended treatment frequency, dosing protocol, maximum acceptance dose for different body parts, maximum number of exposures, follow-up assessment guidelines, etc.
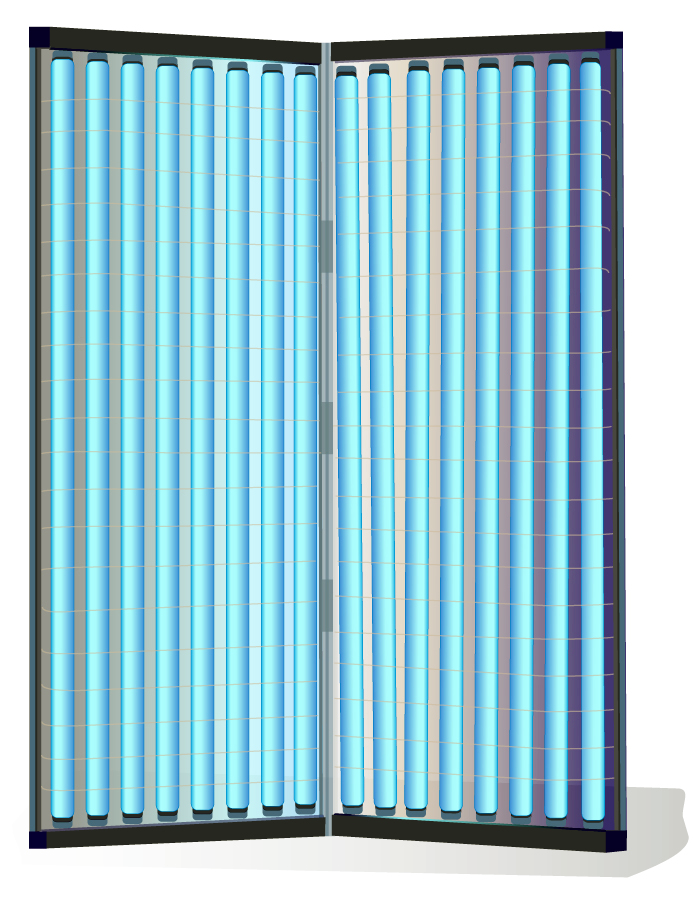
Doctors should determine the duration and progression speed of NB-UVB exposure based on the patient's condition, lesion range, age, and other physical conditions, adjust the treatment plan in a timely manner; concurrently, topical medications can be used to achieve better therapeutic effects.


Source: Vitiligo: Truth, Hope and Change (full-length), 3 Mar 2016, Global Vitiligo Foundation - StepUp4Vitiligo
Topical therapies
Vitiligo is an autoimmune disease, and topical medications mainly achieve anti-inflammatory and immunomodulatory effects. Since the 1950s, topical corticosteroids (TCS) have been the mainstream treatment for vitiligo. They effectively block autoimmune cells from mistakenly attacking epidermal melanocytes, preventing the deterioration and expansion of vitiligo lesions; when used in conjunction with NB-UVB light therapy, it has been clinically shown to effectively cause vitiligo to repigment and maintain. Topical corticosteroids are generally recommended for continuous use for 2-3 months every day; or intermittent use, 15 days of use per month, for a course of 6 months; It is very safe and reliable for patients to follow the doctor's prescription.
Topical calcineurin inhibitors (TCI) are non-steroidal topical drugs, mainly used for the face and neck. They are also first-line treatment drugs for pediatric patients because they are non-steroidal. TCIs are very gentle and safe, without the potential side effect of steroids that may thin the skin. They can also be used in conjunction with TCS and NB-UVB light therapy; the use should be diagnosed by a doctor based on the patient's condition.
Other drug treatments related to vitiligo include: combining NB-UVB treatment with oral methylprednisolone mini-pulse therapy, using 20% topical ethyl vanillate cream to reduce oxidative stress, and using an emulsion with diethylamino hydroxybenzoyl hexyl benzoate and alpha-glucosyl hesperidin as the main ingredients to block other light sources, all to enhance the effectiveness of NB-UVB treatment, and so on.
The aforementioned comprehensive treatment of NB-UVB supplemented with drugs, research shows that more than 75% of vitiligo skin in most patients can achieve repigmentation.
Surgery
Surgical treatments are mostly used for segmental vitiligo (SV), a type of non-generalized vitiligo (V/NSV) mentioned earlier. It shows little sign of spreading, is partly fixed in one location on the body, and the cause of the disease cannot be grasped. After 1 year of NB-UVB treatment for generalized vitiligo (V/NSV), if further progress is desired, surgery may be considered, transplanting melanocytes from healthy skin to vitiligo skin, including: tissue transplantation, cell transplantation, hair follicle transplantation, and transplantation of cultivated epidermal fluid, etc.
Depigmenting treatment
When a patient's overall skin has significantly depigmented (>75%), some will consider permanently depigmenting the remaining normal skin; a famous example is Michael Jackson. Monobenzone (Monobenzyl ether of hydroquinone) is a commonly used medical depigmenting agent and requires a doctor's prescription; there are also other skin bleaching methods such as laser treatment.
The blotchy skin color makes patients look different from ordinary people. Social discrimination and misunderstandings, strange looks/gossip from others, bullying by peers, etc., can all cause great psychological stress and mental distress to patients, especially children and teenagers who are still growing. Doctors should care about the patient's psychological condition, understand the patient's feelings, let the patient understand the causes and treatment methods of vitiligo, the differences before and after treatment, and that treatment time and patience are important. We should encourage patients to actively and patiently accept treatment, and to understand their condition in a positive and optimistic way.
The pathogenesis of vitiligo is complex and varies from person to person. Even though there is still no single drug that can treat all vitiligo at present, we are gradually understanding more about the triggering factors of vitiligo, as well as the different pathogeneses and pathways of autoimmune diseases. Clinical trials have also seen quite encouraging results, and more research is still underway; the future treatment pathways for vitiligo are foreseeable and hopeful.
Reference:
Bergqvist C, Ezzedine K. Vitiligo: A focus on pathogenesis and its therapeutic implications. J Dermatol. 2021 Mar; 48(3):252-270.
Kubelis‑López, D. E., Zapata‑Salazar, N. A., Said‑Fernández, S. L., Sánchez‑Domínguez, C. N., Salinas‑Santander, M. A., Martínez‑Rodríguez, H. G., Vázquez‑Martínez, O. T., Wollina, U., Lotti, T., Ocampo‑Candiani, J."Updates and new medical treatments for vitiligo (Review)". Experimental and Therapeutic Medicine 22.2 (2021): 797.
Mohammad TF, Al-Jamal M, Hamzavi IH, et al. The Vitiligo Working Group recommendations for narrowband ultraviolet B light phototherapy treatment of vitiligo. J Am Acad Dermatol. 2017;76:879–888.
Global Vitiligo Foundation (GVF)(formerly Vitiligo Working Group) - https://globalvitiligofoundation.org/
The NHS website - https://www.nhs.uk/conditions/vitiligo/
Vitiligo Society UK - https://vitiligosociety.org/
The American Vitiligo Research Foundation, Inc.(AVRF) - https://www.avrf.org/
National Vitiligo Bond Inc Foundation - http://vitiligobond.org/